
IFTIM
Imaging Functional and molecular Image processing
Scientific context and objectives
The IFTIM team (Functional and molecular Imaging, and Image Processing) aims to cover two essential areas in clinical imaging: the deployment of new imaging tracers in the preclinical then in the clinic associated with the development of new applications, and the treatment and image analysis. This multidisciplinarity is achieved thanks to a team made up of university hospitalists involved in applied research in medical imaging, biologists and physicists involved in fundamental and applied research in medical imaging and computer scientists specialized in the treatment and analysis of medical images. The team benefits from a very favorable environment for the development of research projects, with in particular the two public health establishments of the Dijon metropolis (CHU and CGFL), thus having a very complete imaging platform and a unique preclinical imaging platform in France.
Team members
Head: Dr. Benoît PRESLES (MCF)
- Dr. J-L. ALBERINI (PU-PH)
- Pr. M. BERHOUMA (PU-PH)
- Dr. A. BOUCHER (MCF)
- Pr. O. BOUCHOT (PU-PH)
- Pr. A. BOZORG-GRAYELI (PU-PH)
- Pr. A. COCHET (PU-PH)
- Dr. A. COURTEAU (IR, UBE)
- Dr. A. LALANDE (MCU-PH)
- Dr. S. LECLERC (MCF)
- Pr. R. LOFFROY (PU-PH)
- Pr. F. MERIAUDEAU (PR)
- Pr. M. MIDULLA (PU-PH)
- Dr. N. PAYAN (IR, CGFL)
- Dr. R. POPOFF (CGFL)
- Pr. G. TRUC (PU-PH)
- Dr. J.-M. VRIGNEAUD (CGFL)
- Pr. M. WALKER (MCU-PH)
Associated Researchers : Dr. O. CHEVALIER, Dr. C. GUIGOU (PH)
Research topics
TOPIC 1 : Multimodal imaging and theranostic
Find out more about our research topics :
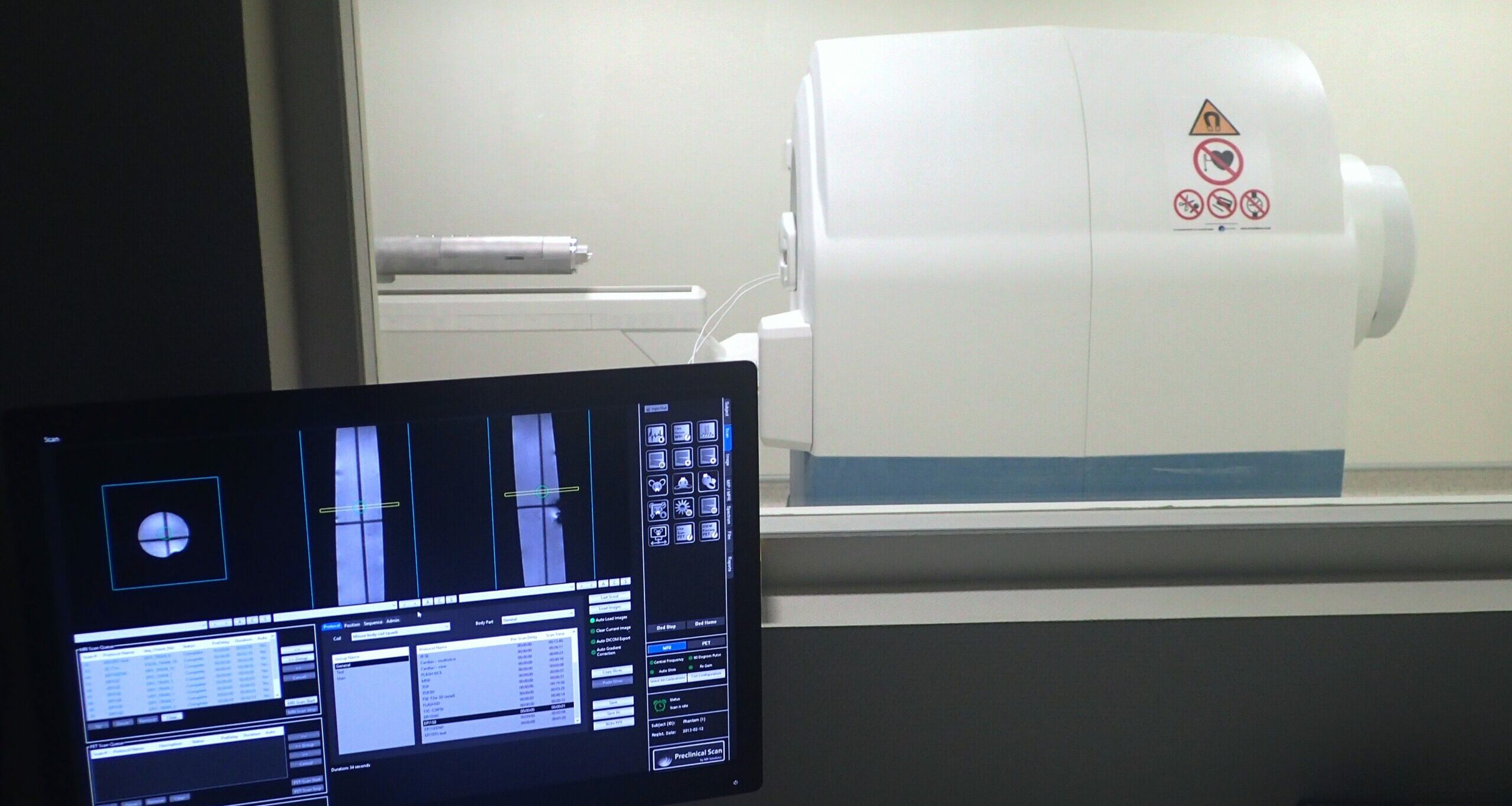
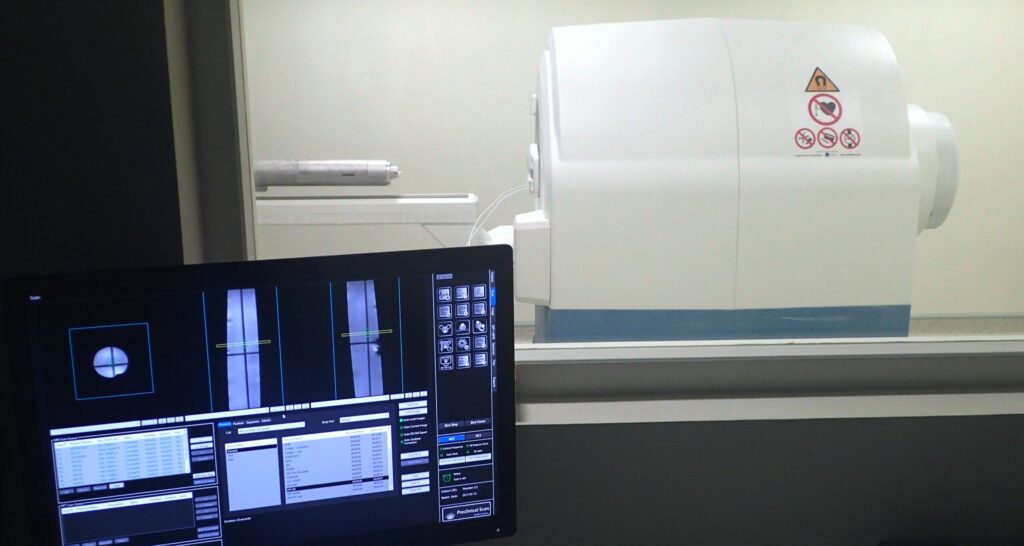
PET/MRI
Led by F. Brunotte and then A. Cochet, the Integrated Magnetic resonance And Positron emission tomography in Preclinical Imaging (IMAPPI – 2012-2024, €7.3m) project has enabled our team to develop a preclinical prototype in Dijon that can simultaneously couple Positron Emission Tomography (PET) and Magnetic Resonance Imaging (MRI). In collaboration with MR Solutions, this project has led to the marketing of a micro-PET/MRI scanner and has provided state-of-the-art scientific equipment (EquipEx) to research teams in Dijon and Biscay, both public and private. The expertise acquired during this project (2012-2024) now enables us to offer advanced solutions for validating the physical performance of nuclear equipment on the CGFL’s preclinical platform, IMATHERA.
We are also committed to improving the quantitative data from imagers (segmentation and attenuation correction in micro-PET/MRI) for dosimetry and cardiac imaging, using the Artificial Intelligence (AI) tools developed by our team members in the other research areas.
Targeted Radionuclide Therapy – clinical translation
Molecular Targeted Radionuclide Therapy (MRT) is a fast-growing therapeutic strategy for the treatment of certain metastatic or locally advanced cancers.
metastatic or locally advanced cancers. It involves the administration of a radiopharmaceutical specifically targeting cancer cells, carrying a radioisotope whose emitted particles (β-, α-particles or Auger electrons) are capable of destroying the cancer cells. IVR also enables a theranostic approach, with the possibility of developing a diagnostic radiopharmaceutical with the same biological behaviour as the therapeutic molecule (companion tracer). The use of this companion tracer makes it possible to verify and quantify the expression of the target in tumours as well as in healthy organs, paving the way for dose adaptation strategies (personalised dosimetry). In addition to its participation in early-phase studies with industrial promotion, our team is positioning itself in this research area with projects ranging from the initial development of new RIV molecules to the implementation of new personalised dosimetry strategies.
Some current examples of projects led or co-lead by our team:
– COMETE: Development of new IVR molecules (and their companion tracer) targeting digestive cancers (pancreatic and colorectal cancers). Preclinical project (ERDF funding) in collaboration with the RITM team and industrial partners (Oncodesign Precision Medicine, Chematech).
– PROFILE: Combining 68Ga-PSMA-11 and 18F-Fluorodeoxyglucose (FDG) PET to plan 177Lu-PSMA-617 treatment for metastatic prostate cancer. Multicentre retrospective study.
– GaLuPro: Evaluation of the concordance between pre-treatment dosimetry performed using 68Ga-PSMA-11 dynamic PET and post-treatment dosimetry of 177Lu-PSMA-617 targeted radionuclide therapy in patients with metastatic prostate cancer resistant to hormonal castration. Single-centre prospective study.
Interventional radiology
Par-de
Image guided surgery
Image-guided surgery is making major advances thanks to developments in augmented reality and artificial intelligence, with applications in several surgical specialities, including ear surgery and carcinological surgery of the oral cavity.
Since 2013, the IFTIM team has been working on a project to develop a new-generation surgical navigation system for ear surgery. This system is based on the superimposition of high-resolution scanner data with the video image of the ear (otoscopy), enabling automatic registration between these two modalities using convolutional neural networks. Camera movements are detected by image analysis algorithms and applied to the scanner data in real time, eliminating the need for motion sensors and human intervention in the registration process. This technology makes it possible to obtain strategic information about the operating scene (targets, trajectories, sensitive structures) and paves the way for the servo-control of surgical robots as well as educational applications.

Resin model of a human temporal bone seen through the Hololens augmented reality headset. The structures of the inner ear (blue) and the vessels (green and red) can be seen from the model’s high-resolution scanner data (Ms Alzein’s M2 project).
In carcinological surgery of the oral cavity, augmented reality could provide a significant advance in the performance of mandibular osteotomies. Bone tumour infiltration is invisible to the naked eye, so surgeons rely on preoperative imaging studies to estimate resection margins. The use of augmented reality, via a Hololens headset or a computer screen, would enable precise visualisation of the section areas, thereby improving the quality of the resection and reducing post-operative functional sequelae. In the reconstruction phase, augmented reality could also optimise the adaptation of fibula flaps to the patient’s anatomy. Artificial intelligence could also simplify registration by eliminating the need for manual selection of anatomical or fiducial markers, making the process faster and more reliable
These advances testify to the transformative potential of image-guided surgery, which improves the precision of interventions and opens up new prospects for personalising surgical care.
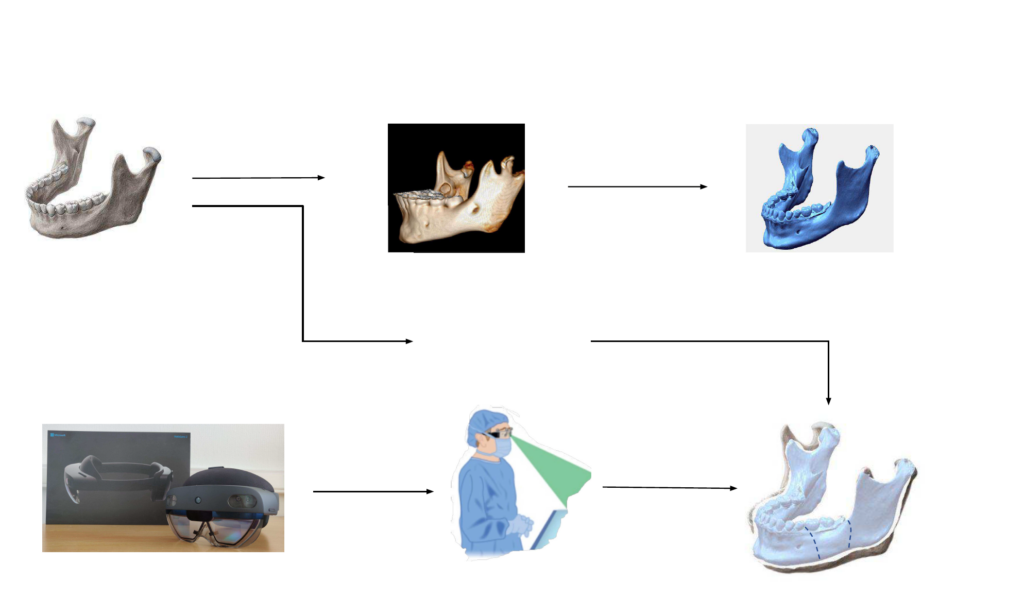
Image guided Radiotherapy
The work of the radiotherapy division, in collaboration with the IFTIM team, mainly focuses on innovation in radiotherapy, particularly in the personalization of treatment. The radiotherapy division promotes the emergence of interdisciplinary projects through a tripartite governance (clinicians, researchers in radiobiology, and medical physics). The research is supported by significant and high-quality resources, notably the MRI-guided ViewRay® accelerator, which enables the development of so-called adaptive radiotherapy and an optimized stereotactic approach.
The projects are organized around two main themes:
Theme 1: Innovative Radiotherapy
MR Linac, AI, quantitative imaging, radiomics, margin personalization, stereotaxy, quality assurance (miniature detectors, adaptive optimization), pseudo-CT.
Theme 2: Combination of Radiotherapy and Systemic Treatments
– Preclinical: radiosensitizing nanoparticles, immunotherapy, evaluation of radiation-induced immune response, biomarker identification.
– Clinical: protocols combining adaptive radiotherapy with nanoparticles or immunotherapies.
Challenges and Perspectives within the IFTIM Team:
– Research efforts around the MR Linac
– Expanding preclinical studies into multicenter clinical trials
– Optimizing the technological platform of the CGFL Radiation Oncology Department (HALCYON® and ETHOS accelerators) to expand the scope of adaptive radiotherapy
– Continuing the integration of radiomics and AI approaches (auto-contouring, data analysis—predictive factors of therapeutic response, pseudo-CT, treatment optimization)
Conclusion:
Participation in the IFTIM team within the CGFL Radiation Oncology Department is part of a multidisciplinary innovation approach. It is driven by a strong dynamic supported by technical, scientific, and clinical expertise, with ambitious projects that hold significant potential for translation into clinical practice.
Main publications – topic 1
- Performance Evaluation and Compatibility Studies of a Compact Preclinical Scanner for Simultaneous PET/MR Imaging at 7 Tesla. A. Courteau, J. McGrath, P. M. Walker, R.Pegg, G.Martin, R. Garipov, P. Doughty, A.Cochet, F. Brunotte, J.-M. Vrigneaud. Trans Med Imaging. 2021;40(1):205-217. doi: 10.1109/TMI.2020.3024722.
- Ethylene-vinyl alcohol copolymer-based non-adhesive liquid embolic agent for transcatheter arterial embolization in patients with abdominal/pelvic arterial bleeding: A prospective, single-arm, multicenter cohort study. Loffroy R, Kobeiter H, Vidal V, Frandon J, Pellerin O, Dean C, Sammoud S, Vernhet-Kovacsik H, Derbel H, Aho-Glélé LS, Chevallier O, Sapoval M. Diagn Interv Imaging. 2025;13:S2211-5684(25) 00009-9. doi:10.1016/j.diii.2025.02.001
- Augmented Reality Based Transmodiolar Cochlear Implantation. C. Guigou, R. Hussain, A. Lalande, A Bozorg Grayeli. Otol Neurotol. 2022;43(2):190-198. doi:10.1097/MAO.0000000000003437
- Randomized phase III trial of metabolic imaging-guided dose escalation of radio-chemotherapy in patients with newly diagnosed glioblastoma (SPECTRO GLIO trial). A. Laprie, G. Noel, L. Chaltiel, G. Truc, MP Sunyach, M. Charissoux, N. Magne, P. Auberdiac, J. Biau, S. Ken, F. Tensaouti, J. Khalifa, I. Sidibe, FE. Roux, L. Vieillevigne, I. Catalaa, S. Boetto, E. Uro-Coste, S. Supiot, V. Bernier, T. Filleron, M. Mounier, M. Poublanc, P. Olivier, JP. Delord, E. Cohen-Jonathan-Moyal. Neuro Oncol. 2024;26(1):153-163. doi: 10.1093/neuonc/noad119.
TOPIC 2 : Medical images processing and IA

Find out more about our research topics :
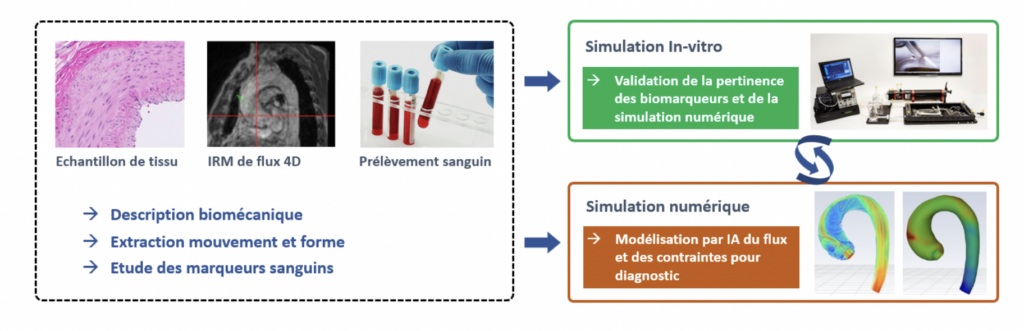
Cardiovascular imaging
Aortic dissection is a serious condition in which a tear in the aorta creates a false channel for blood and can lead to rupture. Imaging alone is not sufficient to assess the risk of progression. The aim of our team’s work, in collaboration with Dijon University Hospital, is to create a digital aortic twin to carry out this monitoring. This simulation will be specific to each patient with a chronic aortic dissection in order to model areas of fragility and detect patients at risk. This modelling will incorporate dynamic imaging data (MRI in particular), clinical, mechanical, histological and biological data (via the study of innovative blood markers). The results obtained in recent years (extraction of biomechanical characteristics from tissue studies, 4D segmentation from MRI, CFD simulation) make it possible to generate this digital twin. This modelling will be generated using artificial intelligence (AI) approaches of the deep learning type, the methods best able to integrate complex processes even when their interactions are not perfectly understood. The modelling will be validated using MRI on aortic phantoms, using an MRI-compatible test bench that simulates heart rhythm. These devices will make it easier to monitor patients and train surgeons.
Radioembolisation of hepatic tumours
Among treatments for unresectable primary liver tumours, radioembolisation or Selective Internal Radiotherapy (SIR) is the locoregional approach of choice. It involves injecting, via the hepatic artery, microspheres loaded with yttrium-90 (⁹⁰Y), a radioelement that is both therapeutic (β- emitter) and imageable in Positron Emission Tomography (PET) (β+ emitter). Prior to treatment, a ‘work-up’ phase combines Magnetic Resonance Imaging (MRI)/Computed Tomography (CT), arteriography and injection of albumin macroaggregates labelled with Technetium-99m (⁹⁹ᵐTc) to simulate the distribution of microspheres and calculate dosimetry. If the indication is confirmed at the multidisciplinary consultation meeting, the microspheres are injected therapeutically, followed by a PET scan. The Dijon Bourgogne University Hospital and the Georges François Leclerc Centre have been working together for more than 10 years to optimise this treatment. The Deep lEarning tooLs for selectIve iNtErnal rAdiation ThErapy of hepatic tumours (DELINEATE) project, conducted with the IFTIM-ICMUB team, aims to personalise RIS using artificial intelligence, advanced dosimetry and simulation, in order to improve its effectiveness while minimising toxicity.
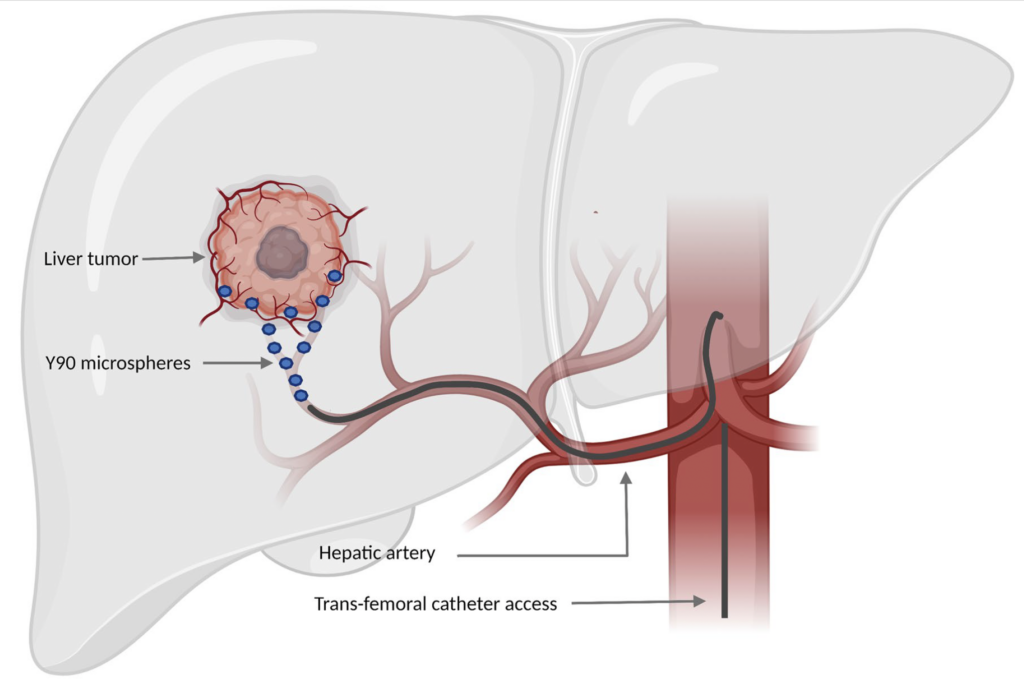
Scheme of injection of 90Y into a liver tumour during RIS treatment. (Image adapted from Vinal et al. 2022)
Retinal imaging
In the retinal imaging theme, we are focusing on two main areas:
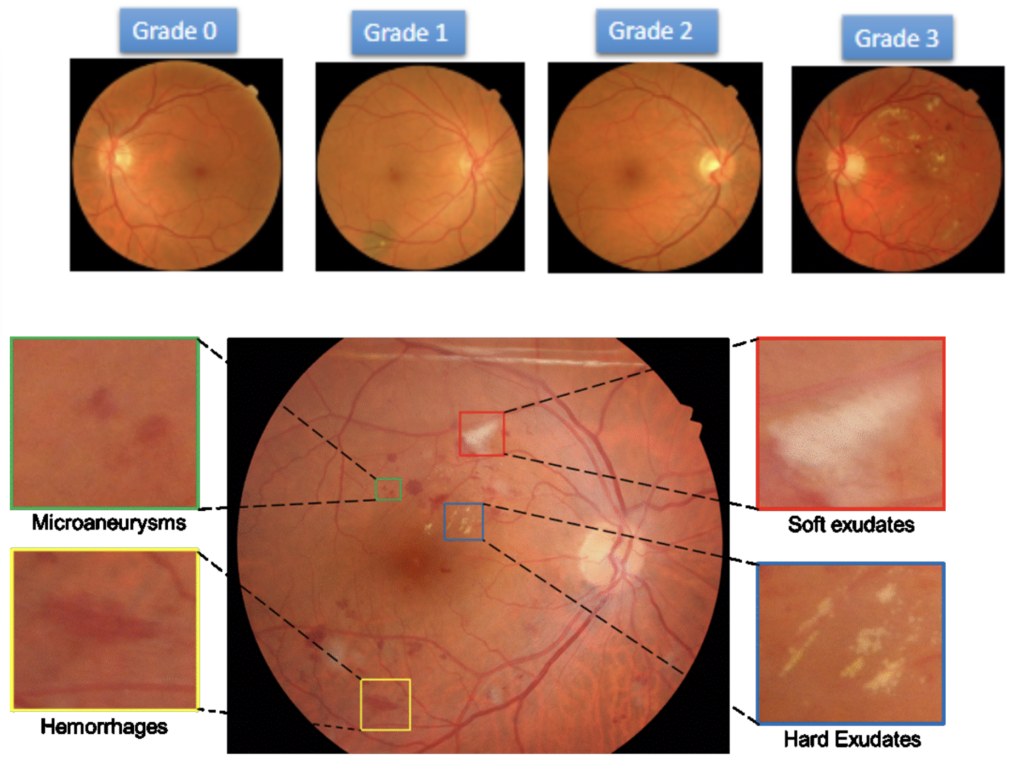
Firstly, we are developing segmentation algorithms using retinography or OCT to measure and identify biomarkers (blood vessels, avascular foveal zone, optic disc, exudates, microaneurysms, etc.) and then to classify retinal pathologies (diabetic retinopathy, AMD, glaucoma, etc.). This theme has led us to organise various academic challenges at leading conferences and to publish in the best journals in the field.
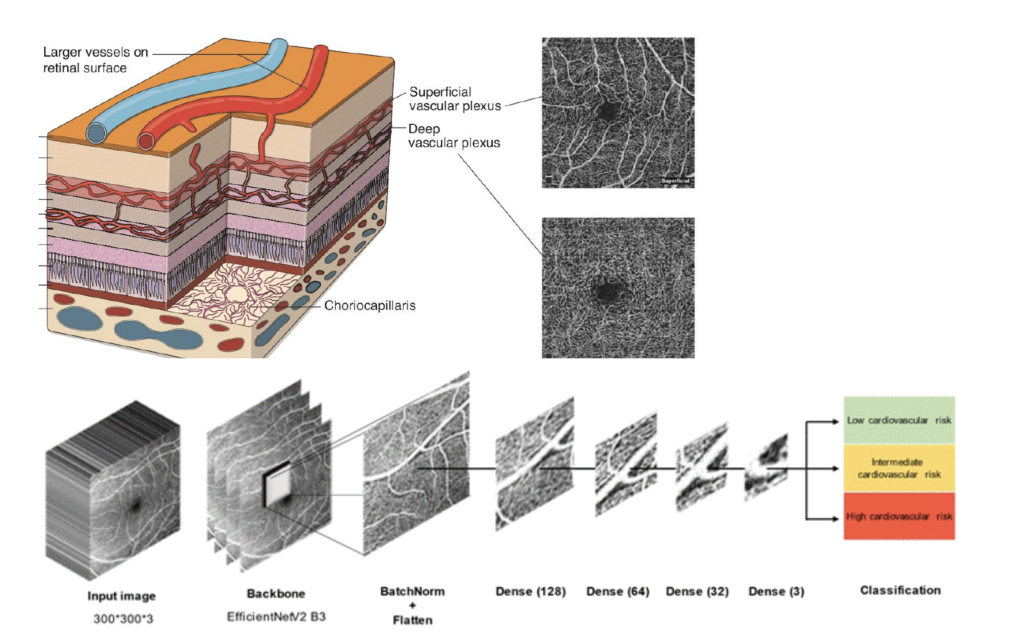
In a second area, in collaboration with the ophthalmology department at Dijon (Pr Creuzot-Garcher and Dr L. Arnould), we are developing prediction algorithms, based on OCTA data, for predicting neuro-cardiovascular risk scores.
Functional and molecular imaging for therapeutic monitoring in oncology
Cancer treatment is undergoing major upheaval with the emergence and development of a host of new therapeutic modalities (targeted therapies such as Antibody Drug Conjugates or Radionuclide therapy, immunotherapy, CAR T-cells, etc.), albeit with inconsistent efficacy and sometimes significant side-effects. It therefore seems essential to develop biomarkers that can be used to establish a prognostic stratification and to assess or even predict the response to a treatment at an early stage, in order to optimise strategies treatment (early change of treatment in case of incomplete tumour response, or on the contrary de-escalation in case of very good response). This biomarker concept is essential for the development of personalised medicine. Our team has acquired considerable expertise in the development of imaging biomarkers, based on the molecular characterisation of tumours before and during treatment, alone or in combination with other biomarkers (clinical, biological, transcriptomic, etc.). Our work is based on the clinical imaging platforms at the CGFL and CHU Dijon (PET/CT including whole-body PET, SPECT, MRI including Magnetic Resonance Spectroscopy, CT including a photon-counting scanner) and the CGFL’s preclinical imaging platform ‘Imathera’ (PET/CT, PET/MRI, SPECT, optical imaging). They are carried out in close collaboration with our clinical colleagues and also with industrial partners, and cover a wide range of pathological situations such as breast cancer, prostate cancer, lung neoplasia, hepatocellular carcinoma, high-grade lymphoma, etc.
A few examples of clinical studies conducted by our team:
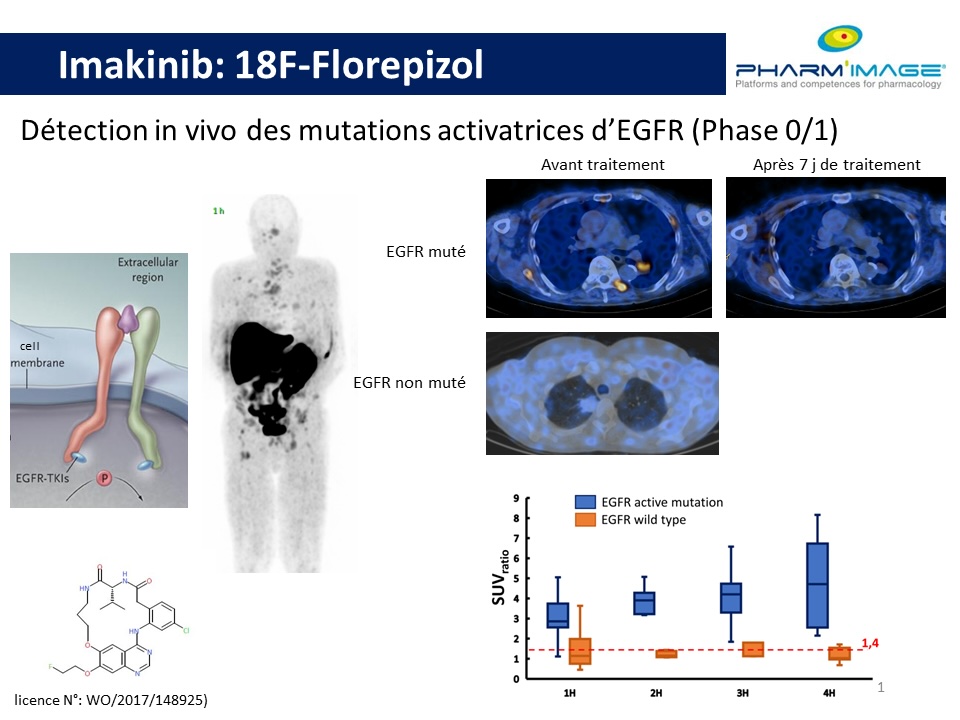
– IMK run 2 (NCT02847377): Development of a new PET tracer, 18F-Florepizol, to detect the presence of activating EGFR mutations in metastatic or locally advanced breast neoplasia. Phase 0/1 study carried out in collaboration with Oncodesign as part of the Pharmimage Economic Interest Group.
– TREN (NCT02386709): 18F-Fluorodeoxyglucose (FDG) PET with dynamic first-pass acquisition for early assessment of response to neoadjuvant treatment of locally advanced breast cancer. Single-centre prospective study.
– ESTROTIMP (NCT05486182): Evaluation of the impact of 18F-Fluoroestradiol (FES) PET on the therapeutic decision in patients with metastatic breast neoplasia treated with letrozole+palbociclib. Multicentre phase IV study conducted in collaboration with General Electric Healthcare.
– PREMETHEP (NCT02847468): Combined use of FDG PET and 18F-FLuorocholine FCH) PET to predict response to sorafenib in patients with advanced hepatocellular carcinoma. Prospective multicentre study (PHRC-K funding).
Main publications – topic 2
- Deep Learning Techniques for Automatic MRI Cardiac Multi-Structures Segmentation and Diagnosis: Is the Problem Solved ? O. Bernard et al. IEEE Transactions on Medical Imaging. 2018;(37):2514-2525. doi: 10.1109/TMI.2018.2837502.
- Navigating the nuances: comparative analysis and hyperparameter optimisation of neural architectures on contrast-enhanced MRI for liver and liver tumour segmentation. F. Quinton, B. Presles, S. Leclerc, G. Nodari, O. Lopez, O. Chevalier, J. Pelligrinelli, JM. Vrigneaud, R. Popoff, F. Mériaudeau, JL Alberini. Sci. Rep. 2024;(14), 3522. https://doi.org/10.1038/s41598-024-53528-9
- IDRiD: Diabetic Retinopathy – Segmentation and Grading Challenge. F. Mériaudeau and coll. Medical Image Analysis. 2020; (56)101561, ISSN 1361-8415. https://doi.org/10.1016/j.media.2019.101561
- Biological correlates of tumor perfusion and its heterogeneity in newly diagnosed breast cancer using dynamic first-pass 18F-FDG PET/CT. N. Payan, B. Presles, F. Brunotte, et al. Eur J Nucl Med Mol Imaging. 2020;(47) 1103-1115. https://doi.org/10.1007/s00259-019-04422-4